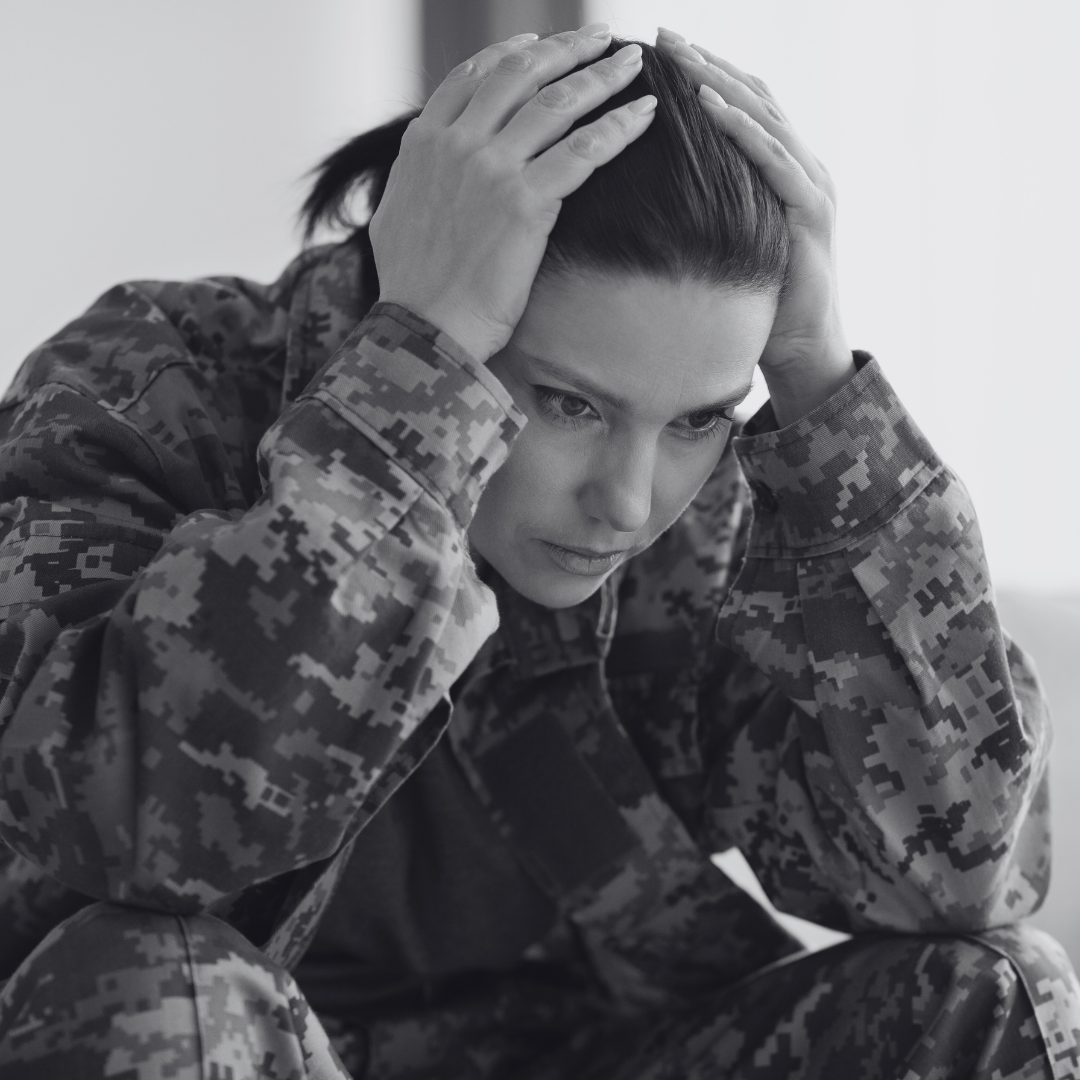
For years, soldiers returning from war carried an invisible burden. In World War I, they called it "shell shock." During World War II, it was known as "combat fatigue." Today, we recognize this condition as Post-Traumatic Stress Disorder (PTSD), which is defined as a mental health condition that arises after experiencing or witnessing a traumatic event.
While PTSD is often associated with military combat—affecting 11-20% of veterans who served in Iraq or Afghanistan—it can stem from any life-altering traumatic event. Car accidents, natural disasters, physical assault, or even witnessing a traumatic event can trigger PTSD. About 8% of Americans will experience PTSD at some point in their lives, with women being twice as likely as men to develop the condition.
Understanding the PTSD Mind
But what exactly happens in the mind of someone with PTSD? To understand this complex condition, imagine your brain as a file cabinet where memories are stored. With PTSD, the traumatic file refuses to stay closed, popping open when you least expect it. People with PTSD often experience vivid flashbacks that make them feel like they're reliving the trauma. While sleeping, nightmares can turn dreams into a battleground.
But PTSD isn't just about flashbacks and nightmares. Anxiety can cause many people to avoid places, activities, or even conversations that remind them of their trauma. They might feel emotionally numb, disconnected from loved ones, or struggle with persistent negative thoughts about themselves or the world. Some people become hypervigilant—always on edge, easily startled, with difficulty concentrating or sleeping.
Breaking New Ground in Treatment
The good news? Significant progress is being made in treating PTSD. Scientists and medical professionals are developing and refining treatments that really work. Three approaches have shown particularly promising results:
- Cognitive Processing Therapy (CPT): This treatment helps patients understand and change how they think about their trauma by reorganizing the cluttered file cabinet in the brain—removing misplaced, damaged files that represent distorted thoughts and replacing them with carefully labeled, accurate documents that reflect a more balanced perspective.
- Prolonged Exposure Therapy: By helping individuals face their fears in a controlled environment, this therapy is akin to gradually turning up the lights in a dark room until the shadows no longer seem threatening.
- Eye Movement Desensitization and Reprocessing (EMDR): This innovative therapy helps people process traumatic memories while focusing on side-to-side eye movements or other forms of bilateral stimulation.
In addition to these 3 approaches, the VA's National Center for PTSD continues to pioneer new approaches to treatment and support such as tools like the PTSD Coach app, providing immediate access to coping strategies. Their research extends from practical interventions—such as service dogs and meditation—to cutting-edge scientific investigations into PTSD's genetic and neurochemical markers. These studies may lead to more targeted treatments and potential preventive measures for high-risk individuals, including combat personnel and emergency service workers.
A Message of Hope
For many people diagnosed with PTSD, the future can bring positive change and healing. When individuals receive professional help roughly 30% find complete relief from their symptoms, while another 40% experience significant improvement despite some symptoms persisting. Even without formal treatment, some individuals may notice their symptoms becoming less severe over time, especially with strong emotional support from family and friends.
Each person's recovery journey is unique - some may find relief within months, while others require more time to develop effective coping strategies. The key message is that improvement and healing are possible, regardless of where someone is in their journey with PTSD. Taking that first step to seek support, whether through mental health professionals or trusted loved ones, can open the door to improved quality of life and lasting recovery.
To learn more, take a deeper dive into the resource materials used for this article:
https://www.research.va.gov/topics/ptsd.cfm
PTSD (Post-Traumatic Stress Disorder): Symptoms & Treatment
Support Resources:
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264,
text “helpline” to 62640, or chat online. In a crisis, call or text 988 (24/7).
For Military Personnel: To discuss treatment options and support resources contact your local VA facility or explore self-help materials at the National Center for PTSD website. www.ptsd.va.gov